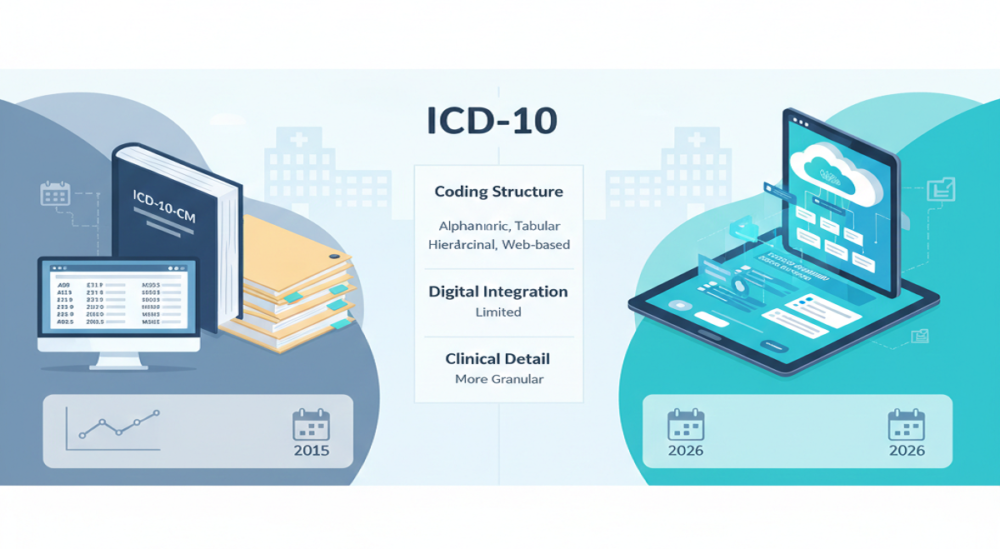
If you survived the ICD-10 rollout, you probably don’t want to hear about another coding overhaul. It took months of training, system updates, and claim monitoring to stabilize things. Now, ICD-11 has been live globally since 2022, and people keep asking the same question: Is the US next?
As of 2026, ICD-10-CM is still the billing standard for US claims. Nothing has changed there. But ICD-11 isn’t just a bigger code book. It’s built differently. And if it eventually reaches US reimbursement systems, the impact won’t be minor.
Let’s break down what’s actually different.
ICD-11 vs ICD-10: The Structural Difference
ICD-10 follows a strict hierarchy. Codes expand using set subcategories, usually ending in .0 through .9. Once those slots are filled, that’s it. Adding more detail often means creating entirely new codes.
ICD-11 removes that limitation.
It does not have a strict structure but instead a base code with optional extension codes. This strategy is referred to as postcoordination. It enables coders to add additional information, such as severity, location, or other aspects, without producing infinite new base codes.
Here’s a simple comparison:
| Feature | ICD-10 | ICD-11 |
| Code Count | 10,607 base codes | 14,622 base codes |
| Structure | Fixed hierarchy | Flexible base + extensions |
| Detail Expansion | Limited | Unlimited combinations |
| Digital Design | Basic structure | Built for digital systems |
That flexibility makes ICD-11 feel more modern. It’s designed for electronic health systems, not paper manuals.
What Is Postcoordination?
Postcoordination is a technical term, and the concept is quite straightforward. Rather than using a single code to represent all possible variations of a condition, ICD-11 allows you to begin with a primary diagnosis and then add extension codes to convey details.
As an example, where you have to use different codes to represent mild, moderate, and severe variations of the same condition, you can add severity as an extension. It makes the underlying system cleaner and more detailed.
That said, more detail means more responsibility. Documentation must clearly support whatever extensions are added.
How Coding Specificity Changes
ICD-11 increases detail in areas that were limited under ICD-10. Rare genetic disorders get clearer representation. Injury coding allows better identification of the object involved. Cancer staging and fracture sites become more precise. Social determinants of health receive stronger classification.
For public health tracking and research, that’s a win. For billing teams, it means documentation can’t be vague. If the code allows more detail, auditors may expect it. Providers may need better note-taking habits to match the expanded structure.
How Disease Classifications Shift in ICD-11
Some of the changes aren’t about adding code. They’re about moving them. Stroke shifts from circulatory diseases into the nervous system chapter. Transient ischemic attacks and silent infarcts sit in the same block.
Allergy conditions move into the immune system chapter. Sleep disorders now live under one unified “sleep-wake” section. The old organic versus non-organic split disappears.
Mental health coding also changes. ICD-11 removes the older distinction between organic and non-organic mental disorders. Certain conditions now require documentation of distress or behavior before classification.
If the US adopts ICD-11, coders will need to retrain their mental map of where diagnoses belong.
Is ICD-11 Active in the US?
No.
ICD-10-CM remains the required diagnosis coding system for billing in 2026. CMS has not adopted ICD-11. However, ICD-11 has been active globally since January 2022 under the World Health Organization. Mapping research continues to evaluate how ICD-10-CM codes align with ICD-11.
Current studies suggest about 60 percent of ICD-10-CM codes can be mapped using ICD-11’s structure and extensions. That means transition wouldn’t be clean, but it wouldn’t start from zero either.
Still, no federal timeline has been confirmed.
What Happens to DRGs and Risk Adjustment?
This is where things get serious.
Diagnosis-Related Groups rely on how diagnoses interact with procedures and comorbidities. Medicare Advantage risk adjustment models also depend heavily on diagnosis coding. If ICD-11 replaces ICD-10-CM, DRG grouping logic would need recalibration. Risk scoring models would require redesign.
Even small structural changes can shift reimbursement weighting. For hospitals and large practices, this could temporarily affect revenue projections. Finance teams would need modeling support during the transition.
This is one reason adoption discussions move slowly. The downstream impact is significant.
Documentation Will Matter Even More
ICD-11 allows more specificity. That doesn’t mean coders can invent details.
If providers document “fracture,” but ICD-11 allows precise anatomical classification, that detail must exist in the chart. Stronger coding systems increase pressure on documentation quality. Training physicians early would reduce the risk of denial if the transition occurs.
Should Providers Start Preparing Now?
There’s no immediate billing shift, so no reason to panic. But ignoring ICD-11 entirely isn’t wise either.
Billing leaders can start by monitoring CMS updates. Coding managers can review structural differences. IT teams can confirm whether EHR vendors support ICD-11 mapping tools. Early awareness costs little. Last-minute reaction costs much more.
Bottom Line for US Providers in 2026
- ICD-10-CM remains active. Claims are still submitted under that structure.
- ICD-11 introduces a flexible coding model with extension codes and deeper specificity.
- Chapter reorganizations reflect updated clinical thinking.
If adopted in the US, reimbursement models, DRGs, and risk adjustment systems would require adjustments. Preparation now doesn’t mean changing your workflow. It means staying informed.
For organizations that want guidance on coding updates, documentation improvement, and long-term transition planning, Rapid RCM Solutions works with US providers to strengthen revenue processes while preparing for system changes ahead.
Coding systems evolve. Revenue protection comes from staying one step ahead, not scrambling after the switch.