Ever had a claim come back denied because of a tiny coding mistake? It’s really frustrating. One small slip, and suddenly you’re dealing with delayed payments, extra work for your billing team, and a stack of rejections that could have been avoided. Modifier 57 is one of those tricky little codes that often trips people up. But when you know how to use it correctly, it protects your reimbursement and keeps audits at bay.
So, what is modifier 57, really? It’s a code you add to an E/M service to show that your evaluation led directly to a major surgical procedure with a 90-day global period. Skip it—or use it wrong—and payers might bundle the visit into the surgery and deny your claim. Get it right, and you’re more likely to get paid fairly for the time and expertise you provided.
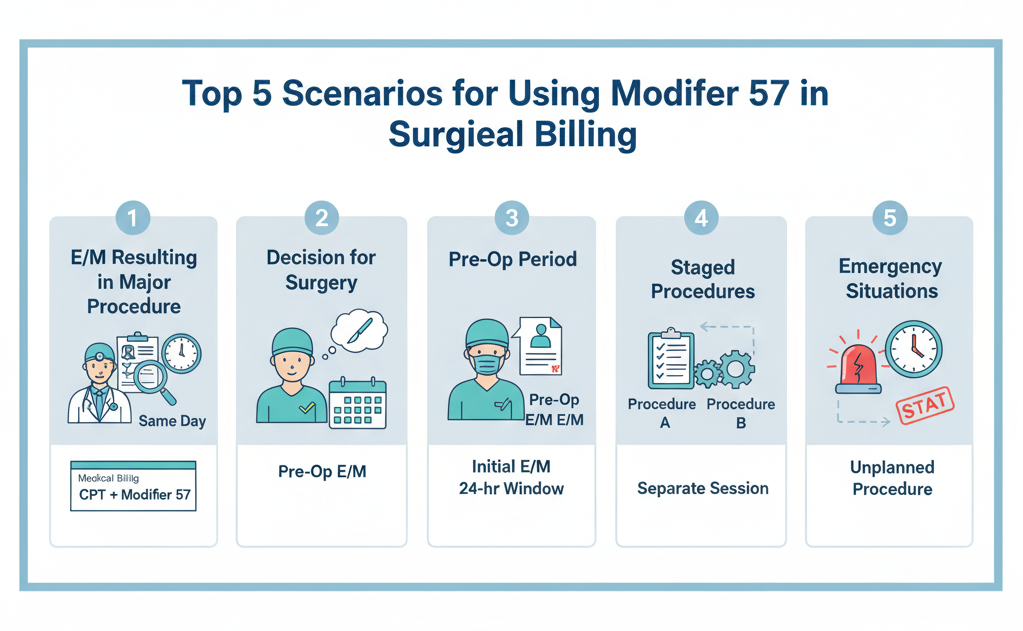
To illustrate this, we will consider five practical instances in which modifier 57 is used. At the end, you will be able to use it perfectly at the right time and place without questioning yourself.
Scenario 1: Emergency Appendectomy in the ER
A patient storms into the ER with severe abdominal pain. The doctor examines them, orders labs, and quickly determines it’s acute appendicitis. The decision? Perform an emergency appendectomy that same day (CPT 44950).
Here, the E/M code, say 99284, gets billed with modifier 57. Why? Because that evaluation led directly to a major surgical decision. If you skip it, the payer might deny the claim for the E/M service, saying it’s included in the surgery.
Think about it: every minute you spend diagnosing and deciding counts. Modifier 57 ensures your work gets recognized.
Scenario 2: Hip Replacement Decision
An aged patient is experiencing deteriorating hip pains. They see an orthopedic surgeon who evaluates them, studies imaging, and concludes that they need a hip replacement (CPT 27130). The following day is the day of the surgery.
Even though the operation isn’t performed on the same day, the E/M visit (for example, 99205) is billed with modifier 57. The rule? The decision must happen on the same day or the day before the surgery. That’s it. Simple, right?
This scenario is common in orthopedic practices. It’s easy to overlook modifier 57 when the surgery is scheduled for the next day, but that’s exactly when it’s needed.
Scenario 3: Postpartum Hemorrhage Leading to Emergency Hysterectomy
After delivery, a woman shows up at the ER with unusual bleeding. The doctor promptly examines her, makes a diagnosis of postpartum bleeding, and concludes that she needs an emergency hysterectomy (CPT 58150).
A separate E/M code, 99285, with a 57 modifier is used to show that the assessment directly led to urgent surgery. Failure to do this may result in failure to receive a high-risk, time-sensitive evaluation legitimacy reimbursement to your practice.
This is a great example of how modifier 57 isn’t just about elective surgeries, but it’s critical in emergencies.
Scenario 4: Fracture Care Without Surgery
Not every major procedure is surgical. Take a clavicle fracture. A patient sees an orthopedic surgeon, and after reviewing imaging, the doctor decides on non-surgical fracture care (CPT 23505) with a 90-day global period.
Here, the E/M service (99203, for example) still gets modifier 57 because the evaluation led to a major procedural decision. Even without cutting into the patient, your evaluation is recognized, and you get reimbursed properly.
It’s a subtle but important point: modifier 57 isn’t just for the OR. It’s about major decisions, period.
Scenario 5: Immediate CABG Decision
A patient arrives with chest pain. The cardiologist evaluates them, diagnoses severe coronary artery disease, and determines that a coronary artery bypass graft (CABG) is needed immediately.
The E/M visit (99285) gets modifier 57 to show the evaluation led to a major surgical decision. It’s straightforward, but it can be easily missed in high-pressure emergency settings. Don’t let that happen; document clearly and append the modifier.
Common Mistakes to Avoid
Even with clear scenarios, mistakes happen. Watch out for these:
Using it on minor procedures: For anything with a 0- or 10-day global period, use modifier 25 instead.
Applying it too early or too late: Modifier 57 only applies when the surgical decision occurs at that visit or the day before. Routine checkups don’t count.
Weak documentation: Your notes should clearly show that the evaluation led to the major procedure. Ambiguity is a red flag for audits.
Why This Matters for Your Practice
When you are balancing surgeries, ER cases, and a full schedule, you can use proper modifiers to save time, lessen denied claims, and safeguard your revenues. It is not just a coding technicality, but the acknowledgment of the life and death decisions you make day in, day out.
Collaborating with a trusted billing provider will relieve your staff. They would be able to assure that modifier 57 is implemented properly, educate staff to distinguish between modifiers 25 and 57, and protect your practice against audits.
Takeaway
Knowing how to use modifier 57 isn’t just about compliance, but it’s also about getting paid for the work you actually do. From emergency appendectomies to urgent CABG decisions, these five scenarios cover the situations you’re likely to see in real practice.
Get it right. Document clearly. And do not allow simple coding errors to cannibalize your hard-earned revenue. Since claims are clean, then everybody is at gain: your practice, your patients, and your peace of mind.