You wouldn’t think something as straightforward as billing for hip pain could cause payment issues, but it does, often. Medical practices and hospitals across the country are running into coding rejections for one simple reason: lack of specificity. Maybe the laterality isn’t mentioned, or the same vague code is used again and again, even after a diagnosis is clear.
In 2025, payers are paying more attention. If your documentation doesn’t match the code, or if you’re still using placeholder codes long after the patient has a diagnosis, then you’re likely to face denials. And every denied claim takes time, phone calls, and rework to fix.
Let’s walk you through what codes you should be using, what details matter in your documentation, and how to stay ahead of these issues.
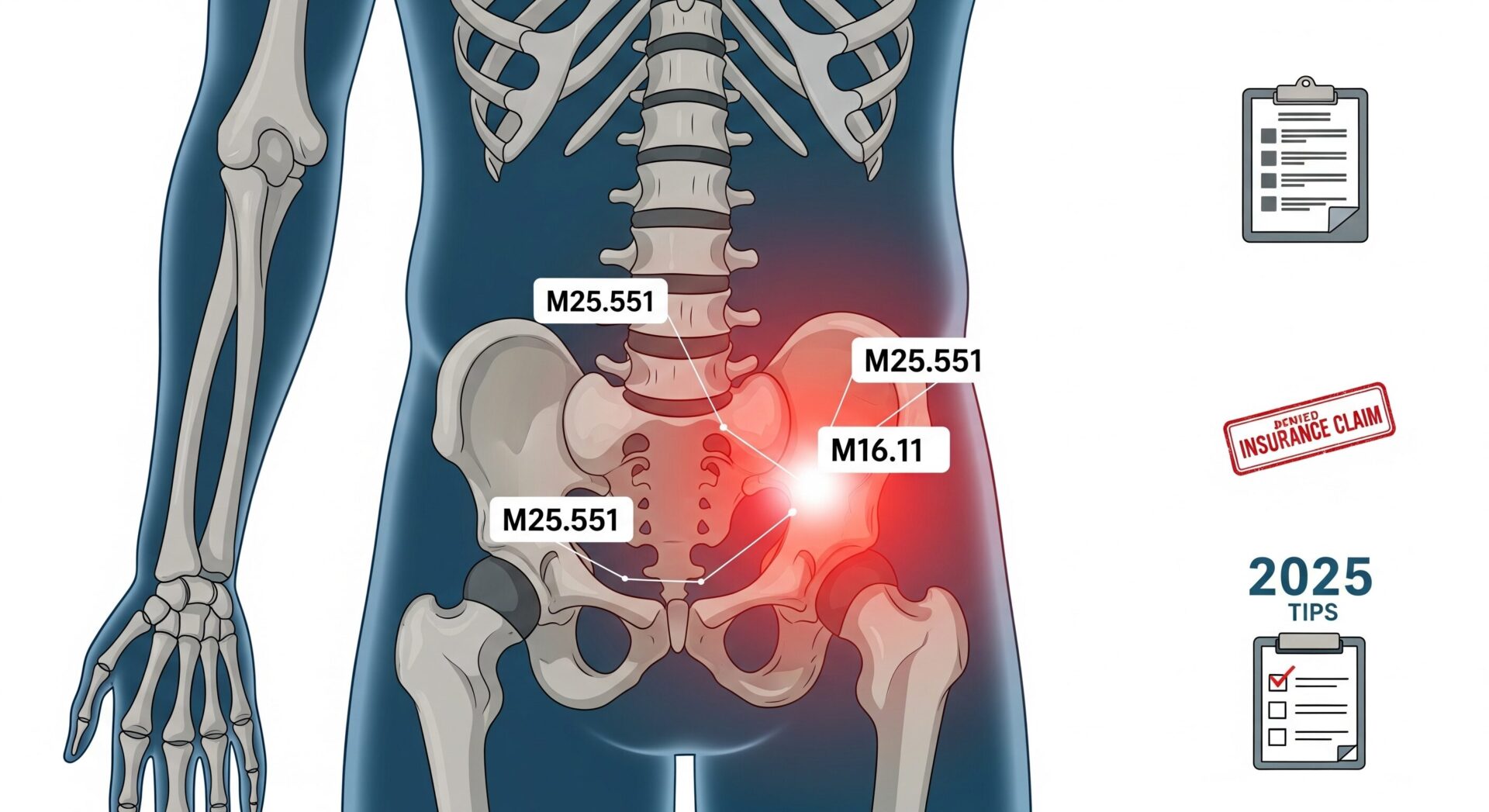
The Most Common ICD 10 Codes for Hip Pain
Here are the standard codes still used most often in 2025:
M25.551 – Pain in right hip
M25.552 – Pain in left hip
M25.559 – Pain in unspecified hip
These are symptom codes. They’re fine when there’s no confirmed cause yet, like at an initial visit. But once you have a diagnosis—like arthritis or a sprain—you should stop using them and switch to something more specific.
A few diagnosis-level codes that often come up:
M16.0 – Bilateral primary osteoarthritis
M16.11 – Unilateral primary osteoarthritis, right hip
S72.001A – Fracture of the right femur (initial encounter)
S73.001A – Right hip sprain (initial)
M54.3 – Sciatica, if the pain is nerve-related
These codes tell payers exactly what’s going on—and they’re more likely to justify services like imaging, injections, or therapy.
Still Using M25.551? Here’s When It’s Okay
There’s nothing wrong with M25.551 if you’re early in the evaluation process. Maybe the patient came in reporting pain in the right hip, but there’s no imaging or physical exam confirmation yet. In that case, the code makes sense.
But if a provider documents arthritis, degeneration, or a known injury, and your claim still uses M25.551, expect trouble. That’s when it becomes a mismatch between what’s in the record and what’s on the claim. It’s a common reason claims are kicked back for “lack of medical necessity.”
Documentation That Actually Holds Up
In 2025, the documentation expectations haven’t just gotten stricter—they’ve gotten smarter. Payers are using automation to review records faster and flag gaps. So here’s what should absolutely be in the note:
- Which side of the body: right, left, or both
- What the pain is from, if known (arthritis, trauma, recovery, etc.)
- How the pain affects mobility, sleep, or activity
- Whether things are improving, worsening, or staying the same
- Any additional diagnoses (like sciatica or post-op complications)
- If the patient isn’t following the care plan, document it. You can even add Z91.19 for noncompliance.
If it’s not in the note, it can’t be backed up—and that’s where denials start stacking up.
Common Errors That Slow Down Reimbursement
Here’s what we’re seeing across hospitals and group practices this year:
- Laterality is missing or doesn’t match the code
- General pain codes are used over and over, even with a diagnosis
- Providers document arthritis, but coders still assign M25.551
- Encounter types are wrong for injuries (like using “initial” on a follow-up)
- Notes don’t reflect the level of complexity being billed
Most of these aren’t big errors, but they’re enough to hold up payment. When you’re handling dozens of claims a day, they add up fast.
One Small Fix = Paid in Full
This happened with one of our clients in spring 2025. A general outpatient clinic submitted a claim using M25.559 for a therapy session. But the therapist had already noted that the patient had right hip osteoarthritis. We caught it, changed the code to M16.11, and resubmitted.
That claim went from denied to paid in four business days.
It’s a good example of how better coding doesn’t mean more complicated coding—it just means aligning the documentation and diagnosis.
Before You Hit Submit: A Quick Checklist
If you’re billing for hip pain, ask yourself:
- Do we know the side? Is it in the note?
- Has the cause been documented?
- Is the ICD-10 code as specific as it could be?
- Do the CPT codes make sense with the diagnosis?
- Are we using the right encounter type?
A short review on the front end can save a lot of work on the back end.
Final Thoughts
Hip pain shows up every day in your patient load. And because it’s common, it’s easy to treat it like low-priority coding. But these “easy” claims are the ones that get denied the most because of small mistakes.
You don’t need to change your entire process—just tighten it up where it counts. Be specific, document clearly, and make sure your coding reflects what’s actually happening with the patient.
Need Help Fixing Denials?
At Rapid RCM Solutions, we work with hospitals and multi-specialty practices to clean up coding issues before claims go out the door. From orthopedic visits to post-surgical care, we help ensure your ICD-10 and CPT coding lines up—so you get paid faster, with fewer resubmissions.
Let’s get your revenue cycle running like it should.
FAQs
What if the patient has ongoing hip pain but no recent injury?
If the pain is chronic and tied to a known condition like arthritis, use diagnosis-specific codes such as M16.11 instead of general symptom codes. It gives payers a clearer picture and supports medical necessity.
How can I double-check my coding before submitting?
Confirm laterality, diagnosis, code specificity, and visit stage.
Can I use M25.551 for follow-ups?
Only if the cause isn’t known yet. Use a diagnosis code once it’s confirmed.