If you’ve ever had a claim denied because of a modifier, you know how small details can create big problems. Modifier 25 and Modifier 59 look simple on paper. In practice, they’re two of the most misunderstood modifiers in medical billing.
The confusion usually shows up after submission. A payer rejects the claim. An audit letter arrives. Or worse, repeated misuse triggers review scrutiny. Denial rates tied to modifier errors can range between 10 and 20 percent. That’s not minor.
Understanding the difference between Modifier 25 and Modifier 59 isn’t optional. It’s part of protecting revenue.
Let’s break this down clearly.
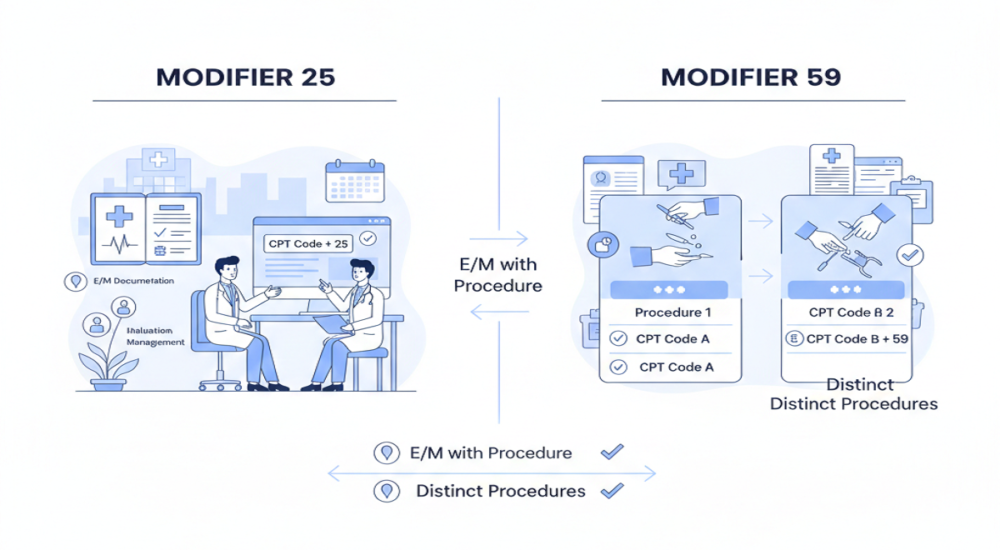
What Is the Main Difference Between Modifier 25 and 59?
Both modifiers help bypass National Correct Coding Initiative (NCCI) edits. But they apply in completely different situations.
Modifier 25 applies only to Evaluation and Management (E/M) codes. It signals that a significant, separately identifiable E/M service occurred on the same day as another procedure.
Modifier 59 applies to procedural codes, not E/M codes. It indicates that a procedure was distinct and should not be bundled under NCCI edits.
One modifies clinical evaluation. The other separates procedures. That distinction matters.
When to Use Modifier 25
Modifier 25 is appended only to E/M codes such as 99202 through 99499. It tells the payer that the provider performed meaningful medical decision-making beyond the usual pre- or post-procedure work.
Routine conversations before an injection don’t qualify. Basic follow-up discussion doesn’t qualify either. There must be separate clinical reasoning. A documented history. A focused exam. Independent decision-making that stands apart from the procedure itself.
For example, a patient comes in for knee pain. The provider evaluates the condition, adjusts treatment, and then administers a therapeutic injection (96372). If the evaluation involved real assessment and decision-making beyond preparing for the injection, Modifier 25 may apply to the E/M code. Without clear documentation, it doesn’t.
When to Use Modifier 59
Modifier 59 applies to procedural codes, not office visits. It signals that two procedures performed on the same day were distinct.
“Distinct” can mean separate anatomical sites, separate sessions, or entirely separate procedures that are normally bundled. For example, if a dermatologist removes two lesions from different sites, Modifier 59 may be appended to the secondary procedure code to show they were separate.
But documentation must support that distinction. Location matters. Time matters. Clinical separation matters. Modifier 59 should never be added to an E/M code.
Side-by-Side Comparison
Here’s a practical comparison to keep things straight:
| Aspect | Modifier 25 | Modifier 59 |
| Applies To | E/M codes only | Procedure codes only |
| Purpose | Separates E/M from procedure | Separates procedures from each other |
| Key Requirement | Distinct medical decision-making | Distinct site, session, or procedure |
| Documentation Needed | Separate exam, history, MDM | Clear site, time, or anatomical proof |
| Example | 99214-25 with injection | 12001-59 for separate incision |
Keeping this chart in mind prevents crossover errors.
CMS and NCCI Guidelines for 2026
Before applying either modifier, check NCCI edits. If a procedure pair is bundled, review whether an appropriate modifier is allowed. Modifier 59 is considered a last resort. CMS prefers more specific X modifiers when applicable.
For example:
- XS indicates a separate structure
- XE indicates a separate encounter
- XP indicates a separate practitioner
- XU indicates unusual non-overlapping service
Payers like BCBS often prefer these X modifiers over 59 because they provide clearer justification. Modifier 25 should never be used to bill routine pre-procedure work. CMS guidance is clear on that point. The E/M must stand on its own.
Modifier 59 misuse, especially when procedures involve the same anatomical region without a clear distinction, often triggers audit reviews.
Common Mistakes That Trigger Denials
The most frequent Modifier 25 error is billing a routine pre-procedure discussion as a separate E/M visit. If the provider simply explains the procedure and proceeds, that does not justify Modifier 25.
Auditors look for documentation that proves a real assessment occurred.
Modifier 59 errors often involve bypassing NCCI edits without sufficient proof. For example, using 59 when two procedures occur in the same region without documented separation. That approach doesn’t hold up in review. When documentation lacks specific anatomical notes or clear timing differences, claims get denied.
Documentation Tips That Protect Claims
For Modifier 25, ensure the note clearly shows:
- Separate history
- Distinct exam findings
- Independent medical decision-making
Avoid vague entries. If the evaluation influenced treatment beyond performing the procedure, that must be clear.
For Modifier 59, document:
- Exact anatomical site
- Distance between lesions if relevant
- Separate incisions if applicable
- Distinct session timing
A note such as “separate incisions 2 cm apart” strengthens support. Details prevent disputes.
Why Payers Watch These Modifiers Closely
Both modifiers increase reimbursement when used correctly. That’s why overuse raises red flags. Payers analyze frequency patterns. High utilization of Modifier 25 or repeated 59 usage in the same specialty draws attention.
Overuse doesn’t always mean fraud, but it increases scrutiny. And scrutiny slows payments. Clean use supported by strong documentation keeps risk low.
Practical Example: Same-Day Injection and Office Visit
A common scenario involves an office visit and injection on the same day.
In case a patient has a new complaint that needs to be thoroughly evaluated and is given an injection, one can use Modifier 25 to the E/M code.
If the visit simply supports giving the injection without a new assessment, Modifier 25 should not be added. For procedural combinations, if two procedures are performed on distinct areas, Modifier 59 may separate them. Context determines the right choice.
Final Thoughts
Modifier 25 and Modifier 59 are not interchangeable. One separates evaluation from procedure. The other procedures are separate and differ from each other.
The difference comes down to documentation and intent. Check NCCI edits first. Use Modifier 25 only when real medical decision-making exists. Use Modifier 59 only when procedural services are clearly distinct. When appropriate, use X modifiers for greater specificity.
Small modifier errors create avoidable denials. Careful review prevents that. For practices that want expert-level claim scrubbing and cleaner submissions, Rapid RCM Solutions helps US providers maintain high clean claim rates while reducing audit risk.
Because when modifiers are used correctly, revenue flows smoothly instead of getting stuck in review.