Billing rarely feels urgent until payments slow down. One day claims are moving, and the next day denials start piling up. Staff get stuck fixing the same issues again and again, while revenue is put on hold. That’s when many practices start questioning how their billing really works. Is the traditional way still enough, or do modern tools actually make things easier?
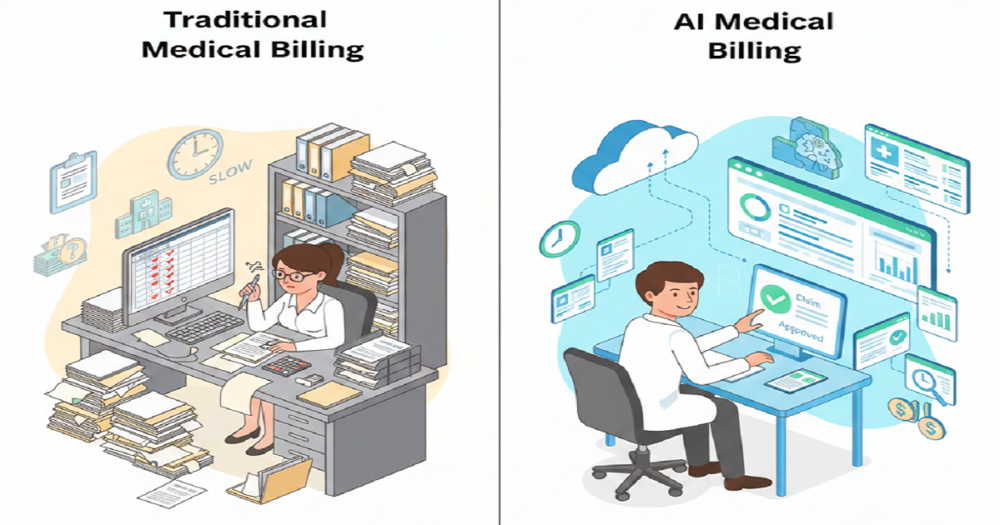
This isn’t about chasing trends or replacing people with machines. It’s about understanding how AI medical billing benefits compare with traditional billing workflows in real, everyday practice life. When you break it down, the differences are easier to see than most people expect.
How Traditional Billing Workflows Operate Day to Day
Traditional billing depends heavily on human effort. Teams review charts, select codes, apply modifiers, double-check payer rules, and submit claims. Most of it’s manual, scattered across different systems. Even the pros have to stay sharp to keep it all straight.
At manageable volumes, this process can work well. Problems start when patient numbers grow or payer rules change. A small mistake can delay a claim for weeks. Fixing it means rework, follow-ups, and more pressure on staff who are already stretched thin.
Where Traditional Billing Begins to Crack
The first crack usually shows up as denials. They don’t arrive all at once. They creep in slowly. A few here, a few there. By the time the pattern becomes clear, revenue has already taken a hit.
Another challenge is visibility. Traditional workflows often spot issues after money is lost, not before. Reports come late. Trends get missed, and billing teams spend their days scrambling to fix problems instead of getting ahead of them. Always playing catch-up just wears people down.
What AI Medical Billing Actually Does
AI medical billing acts as a second pair of eyes. It reviews claims before they go out, catches missing details, coding slip-ups, and any red flags that have caused problems in the past. So you’re not just counting on people to catch everything; AI keeps the process steady.
But it’s not about AI kicking billers out of the picture. It’s there to help. The system takes care of the boring, repetitive stuff, so people can free up their time to handle things like appeals and talking to payers. That balance is what really counts, not just getting things done fast.
Real AI Medical Billing Benefits Practices Notice First
The main thing people notice is that there are way fewer unnecessary mistakes. AI catches problems right away, so claims are cleaner from the start. After a while, you see denials go down and payments show up sooner.
Time’s another big win. The employees do not have to troubleshoot minor mistakes all the time, so there is no stresses and everyone is on schedule. Billing feels more controlled instead of chaotic.
AI also improves clarity. Reports show where problems start, not just where they end. Practices can fix root causes instead of guessing.
Accuracy Compared Side by Side
Traditional billing accuracy depends on attention and experience. Even great teams make mistakes when workloads increase. AI doesn’t get tired or distracted. It applies the same checks every time.
That consistency makes a difference. Claims go out cleaner. Fewer come back unpaid. Accuracy improves without adding extra stress to staff.
Speed and Workflow Efficiency
Manual workflows slow down as volume rises. Each extra claim adds pressure. AI systems scale more smoothly. They review claims quickly without adding strain.
That speed doesn’t feel rushed. It feels steady. Claims move forward without constant interruptions, which keeps the entire workflow flowing better.
Cost and Staffing Impact
Traditional billing may seem cheaper upfront, but hidden costs add up. Rework, delayed payments, overtime, and staff turnover all affect revenue. You will rarely see these costs on a simple budget sheet.
AI billing is an investment that usually reduces long term costs. Reduced denials imply reduced rework. Increased payments enhance cash flows. Staffing becomes more manageable when teams aren’t overwhelmed.
Team Adoption and Change Concerns
Change always brings hesitation. Some staff worry about learning new tools. Others fear losing control. Effective communication alleviates that tension.
When teams see AI as support, not replacement, adoption improves. Training matters. Early wins matter too. Once people see fewer denials and smoother days, confidence grows naturally.
Blending Technology With Human Judgment
AI shines when you team it up with people who are experienced. Let the tech to do the data and trend patterns. People step in for the judgment calls, the context, the conversations.
It’s all about finding the right mix. Practices don’t need to switch everything overnight. Many start small, then expand as comfort grows.
Choosing What Works for Your Practice
Every practice is different. Smaller clinics value simplicity. Larger groups need scale. The right choice depends on volume, goals, and resources.
What matters most is steady payment, clear insight, and manageable workloads. Whether improving traditional workflows or adding AI support, the goal stays the same. Reduce friction. Improve reliability.
Practices before altering anything ought to check on denial trends, staff workload, and cash flow stress. These all signals to what requires attention.
Moving Forward With Clarity
The billing continues to evolve as healthcare becomes increasingly complex. Adaptive practices remain ahead. When you really understand what each method does well (and where it falls short), you make smarter choices.
Rapid RCM Solutions steps in here. Their skilled billing staff, paired with modern tech, helps make billing more accurate and keep payments moving. You get fewer delays, a smoother workflow, and a stronger payment cycle.