Time is one of the few things clinics never have enough of. Every doctor knows how quickly a day can fall apart when something as simple as insurance eligibility isn’t correct. One outdated plan, one missed policy change, one detail that didn’t get verified properly; and suddenly your team is dealing with frustrated patients, rescheduled appointments, and denials that could’ve been avoided entirely. It’s a small slip that creates a long chain of problems.
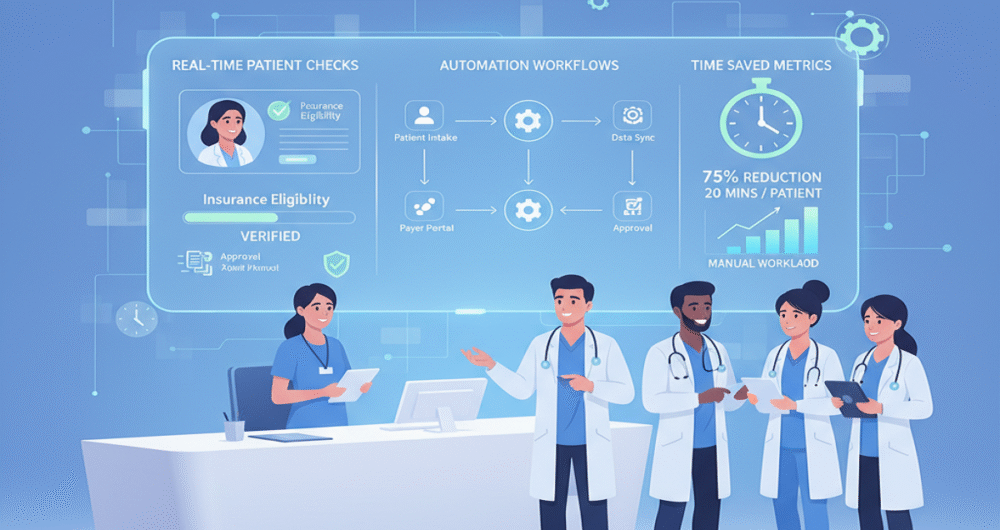
That’s why automated eligibility verification has become such a practical upgrade for clinics. It takes a task your team handles dozens of times a day and turns it into something fast, accurate, and dependable. You don’t need to spend hours checking coverage in a manual way. Your practice will get real-time information without any hectic.
For doctors running busy schedules, this isn’t a luxury. It’s a time saver that makes the entire workflow smoother, from the front desk to the billing department to the exam room.
Manual Checks Slow Down Your Staff More Than You Think
Most clinics underestimate how much time manual eligibility eats up. Every check requires logging into payer portals, searching member IDs, reviewing benefits line by line, and sometimes calling the insurance company directly. When your staff repeats this process for every patient, the workload adds up quickly.
The problem isn’t that your team can’t handle it. The problem is that it pulls them away from tasks that actually support patient care. Manual checks interrupt check-in, delay schedules, and force staff to multitask in ways that aren’t sustainable.
Automated eligibility verification removes that bottleneck. It gives your staff accurate information before the patient arrives, which keeps your day moving without unnecessary slowdowns.
Real-Time Accuracy Prevents Last-Minute Problems
One of the biggest frustrations for clinics is discovering insurance changes at the wrong time, usually right when the patient is sitting in front of you. A plan renews, benefits shift, a deductible resets, or coverage ends earlier than expected. These issues aren’t always predictable, and they create delays when you find out too late.
Automated verification updates benefits in real time. Your team gets the latest info on coverage, copays, coinsurance, deductibles, and visit-specific needs. This lets you decide things before the appointment, so you don’t get stuck with denied claims later.
When eligibility is accurate from the start, you avoid unnecessary back-and-forth with payers and prevent the follow-up workload that normally lands on your billing team.
Your Staff Gets a Noticeable Amount of Time Back
Front desk staff are the first point of contact for patients, and their workload is heavy even without manual eligibility tasks. They handle check-ins, answer phones, deal with scheduling issues, cancellations, and all sorts of patient questions – often juggling it all at once.
Automated eligibility takes one of the biggest time-consuming tasks off their plate. Instead of searching multiple portals, refreshing pages, or calling insurers, your team gets the information instantly. It reduces interruptions and allows them to focus on delivering a smoother check-in experience.
For many clinics, automated eligibility saves hours every single day. Multiply that across a month, and it easily reaches hundreds of hours that your staff can redirect toward patient needs instead of administrative work.
Preventable Denials Drop Dramatically
Eligibility-related denials are some of the most common issues clinics face. They’re also among the most preventable. A simple mistake, an inactive plan, the wrong payer selected, or outdated benefits can push a clean claim into a denial category.
Automated eligibility reduces those errors significantly. Claims go out correctly every time, so you get paid faster. Plus, your billing staff doesn’t waste time on issues that could have been avoided. It creates a more predictable revenue cycle, which helps your clinic stay financially steady.
Doctors don’t need to deal with reimbursement delays caused by something that could’ve been corrected upfront. Automation removes that risk.
Patients Appreciate Clear Information Upfront
Patients are more informed than ever, but insurance still confuses most people. When they’re told one amount during check-in and see a completely different figure later, it affects trust immediately.
Automated eligibility allows your staff to give patients accurate information from the start. It can clearly explain your expected copays, what’s left on your deductible, and coverage details, so there are fewer misunderstandings and less stress about money.
Knowing what your plan covers before you come in will make you feel more at ease and ready. This also makes you happier and prevents uncomfortable talks down the road.
Your Team Makes Fewer Errors and Works More Efficiently
When the process is rushed and repetitive, it is easy to make errors. Manual verification enhances the likelihood of inaccurate data input, old data, or failure to receive updates from the payer. These mistakes do not simply lead to denials; they also bring more administrative workload in the future.
Automated eligibility provides clean, accurate data right away. Your staff doesn’t need to repeat the same checks multiple times or review complicated benefit structures manually. This reduces burnout, improves morale, and helps your team work at a steady pace instead of constantly trying to catch up.
Your Daily Workflow Becomes Predictable and Stable
A clinic will work well when an orderly schedule is in place. The problem of eligibility interferes with that flow even more than many think. A single mistake in coverage can upset your whole morning.
The process is predictable with automation. Before your first patient, your team already knows that the coverage has been secured. They are not rushing to resolve unforeseen problems, postponing appointments, or attempting to fit in last-minute verification calls.
Predictability assists physicians to remain focused, patients to move, and the operational rhythm to be cleaner during the day.
It’s a Small Change That Makes a Noticeable Difference
Automated eligibility verification might sound like a small change, but it really helps clinics out a lot. It makes check-in faster, fixes mistakes quicker, stops claims from getting turned down, and lets staff spend more time with patients instead of being stuck with paperwork.
It’s one of the few process improvements that saves time, reduces stress, and improves accuracy all at once. For practices looking to streamline operations without disrupting their workflow, this is one of the easiest and most practical changes to make.
Conclusion
Automated eligibility verification is not technology to the power of technology. It is about providing clinics with an opportunity to work more effectively without compromising the accuracy or patient satisfaction. Practices eliminate manual processes and reduce errors that can be avoided, save time, enhance communication, and provide a more enjoyable experience to staff and patients.
With automated management of eligibility, your clinic operates more efficiently, smoothly, and without delays, and the time saved is rapidly accumulated.